Translate this page into:
Osteolytic change surrounding biodegradable cement restrictors used in total hip replacements mimicking malignancy

*Corresponding author: Rajesh Botchu, Department of Radiology, Royal Orthopedic Hospital, Birmingham, United Kingdom. drrajeshb@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Ariyaratne S, Davies M, Evans S, James S, Botchu R. Osteolytic change surrounding biodegradable cement restrictors used in total hip replacements mimicking malignancy. Indian J Musculoskelet Radiol. 2024;6:28-32. doi: 10.25259/IJMSR_50_2023
Abstract
Peri-prosthetic osteolysis is a well-documented complication of total hip arthroplasty. A lesser-known form of peri-prosthetic osteolysis occurs specifically involving biodegradable cement restrictor devices which may be used in total hip replacements (THRs) to contain the cement material within the femoral medullary canal, which would help maintain adequate pressurization within the canal and secure the prosthetic femoral stem. The device is inserted into the femoral medullary canal just distal to the prosthetic stem. Different types of restrictors are used; certain biodegradables forms of restrictors are known to cause progressive osteolysis at the site of insertion, which can present as a gradually enlarging focal lytic lesion on imaging. While this entity as well as its relevance as a risk factor for peri-prosthetic fracture has been discussed in existing literature, the resemblance of this entity to a neoplastic process, particularly given the gradual enlargement over time is not well-documented. Understanding this process and potential pitfall when interpreting imaging, particularly X-rays, in patients who have previously undergone a THR, is important to avoid misdiagnosis of this otherwise benign entity as a neoplastic process and would potentially negate the need for unnecessary investigations.
Keywords
Total hip replacement
Osteolytic change
Lytic lesion
Neoplasm
Cement restrictor
INTRODUCTION
Total hip arthroplasty is a commonly performed procedure worldwide. A cement restrictor is an intramedullary device inserted into the medullary canal distal to the femoral stem in total hip arthroplasty procedures to maintain adequate pressurization within the medullary canal. The sealing of the canal from the device also prevents excess seepage of cement into the distal medullary canal.[1] Some of these devices are biodegradable, and over time, these cement restrictors can progressively degrade, resulting in osteolysis at their site of insertion. This may be seen as a focal lucency on X-rays.
Osteolytic change involving biodegradable osseous implants is a known entity[2] that has been described in several publications. In a study published by Hanssen et al.,[3], which analyzed a cohort of 284 patients with total hip arthroplasties, 25 were found to have substantial osteolysis, and a further 19 were found to have severe osteolysis surrounding the restrictor plug. In addition to the osteolysis, several other complications related to these restrictors have been described, ranging from adverse reactions to the material, prosthesis loosening, and peri-prosthetic fractures.[4,5] However, the possibility of this entity mimicking neoplasia, as well as its implications, is sparsely discussed in the existing literature.
We describe two cases of patients presenting with distal periprosthetic osteolytic lesions on X-rays in the setting of prior total hip arthroplasty. On both occasions, the presence of background risk factors and clinical suspicion of malignancy resulted in these lesions being investigated to exclude the possibility of malignancy. One of the patients underwent a biopsy of the lesion, which confirmed the benign nature of the lesion.
This paper aims to make the reader aware of this potential pitfall. It stresses the need for consideration of this entity when presented with a lytic lesion adjacent to the femoral stem in a patient with prior THR, particularly when there are other predisposing risk factors raising suspicion for an osseous neoplastic process.
CASE SERIES
Case 1
An 81-year-old female who had a cemented left total hip replacement (THR) inserted 11 years prior for treatment of osteoarthritis presented with left hip pain. Radiographs obtained one year apart demonstrated an enlarging expansile lytic lesion at the tip of her cemented femoral stem [Figure 1a and b]. There was no imaging of the hip before this. Her preliminary biochemical screens for malignancy, including a myeloma screen, were negative, and she had normal inflammatory markers.
![Anteroposterior radiographs radiographs (a,b) one year apart (most recent [b]) demonstrating a gradually expanding lytic lesion of the left femoral diaphysis adjacent to the prosthetic femoral stem (white arrows).](/content/107/2024/6/1/img/IJMSR-6-028-g001.png)
- Anteroposterior radiographs radiographs (a,b) one year apart (most recent [b]) demonstrating a gradually expanding lytic lesion of the left femoral diaphysis adjacent to the prosthetic femoral stem (white arrows).
A magnetic resonance imaging (MRI) scan and a computed tomography (CT) scan demonstrated a fluid-filled cavity at the tip of the left femoral stem with endosteal scalloping [Figures 2a-c]. The lesion demonstrated low T1 and high T2 signal on MRI. There was no significant uptake seen in this region on bone scan. While the findings were thought to be related to a complication of the hip replacement, the progressive increase in the size of the lesion raised concerns about the possibility of a neoplastic process; hence, a decision was made to proceed with a biopsy. A core biopsy of the lytic lesion was performed using an 8-gauge Jamshidi™ bone biopsy needle.
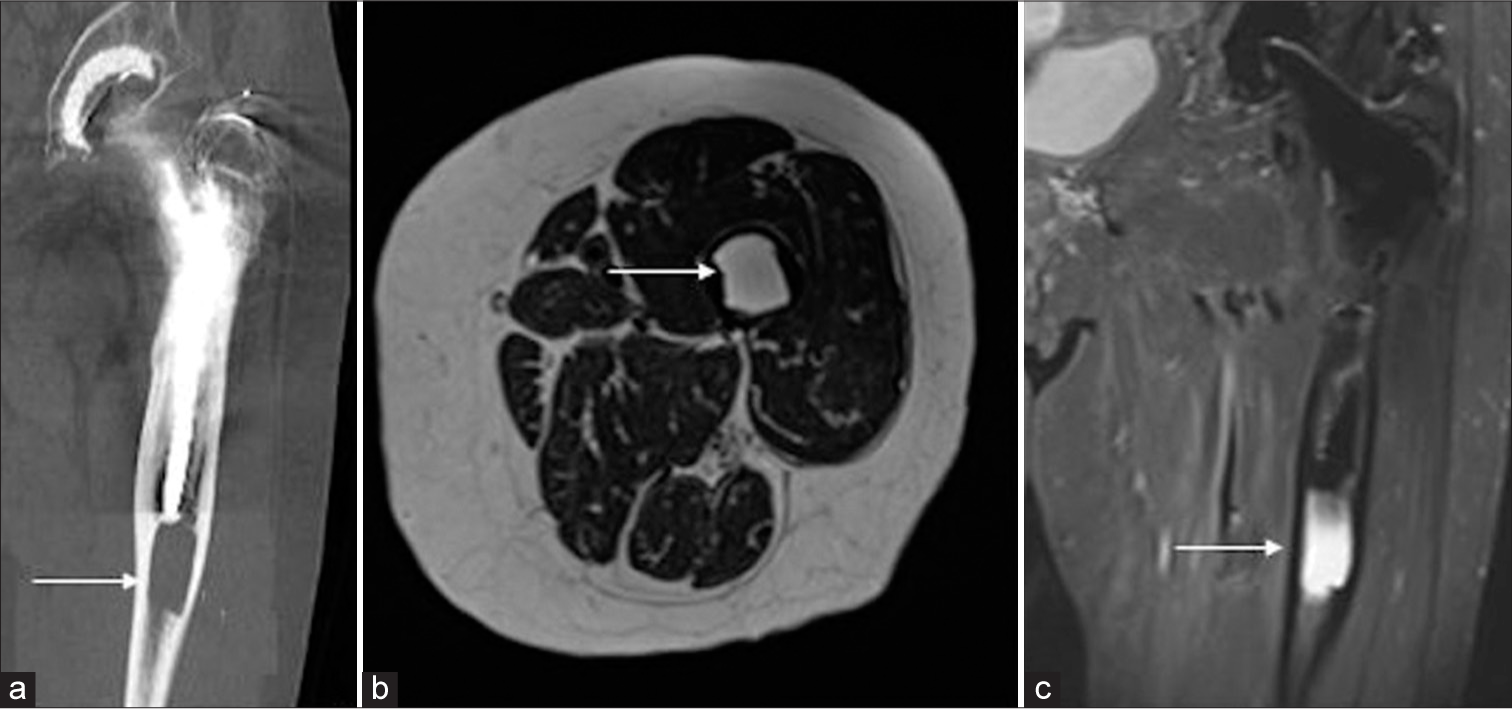
- (a) Computed tomography coronal (white arrow) and (b) magnetic resonance imaging axial T2 (white arrow) and (c) coronal T2 FS sequences demonstrating the lytic lesion (white arrow).
Histology of the biopsy sample revealed non-specific findings with some inflammatory cells, but there was no evidence of malignancy or neoplastic process. There was no evidence of infection on microscopy and culture. The patient was reassured of the likelihood of this lesion being related to the prosthesis and was discharged.
Case 2
A 91-year-old female presented with ongoing right hip pain. She had a prior history of right THR 13 years ago for treatment of osteoarthritis. A preliminary X-ray was obtained, which demonstrated a lytic lesion adjacent to the prosthetic right femoral stem. Considering these findings, a myeloma screen was conducted, which revealed polyclonal Kappa light chains in the urine.
X-rays of the right hip at presentation [Figure 3] show a lytic lesion in the right mid-femoral diaphysis adjacent to and immediately distal to the prosthetic femoral stem. The lesion was centered within the medullary cavity, with scalloping of the adjacent cortex. MRI confirmed the finding of an intramedullary lesion with cortical scalloping, demonstrating high T2 and proton density signal and low T1 signal [Figures 4a-c]. The findings raised concern for a neoplastic process, the most common differentials for an osseous lytic lesion in this age group being metastasis and multiple myeloma.[6] The latter was of particular concern, given the biochemical findings.
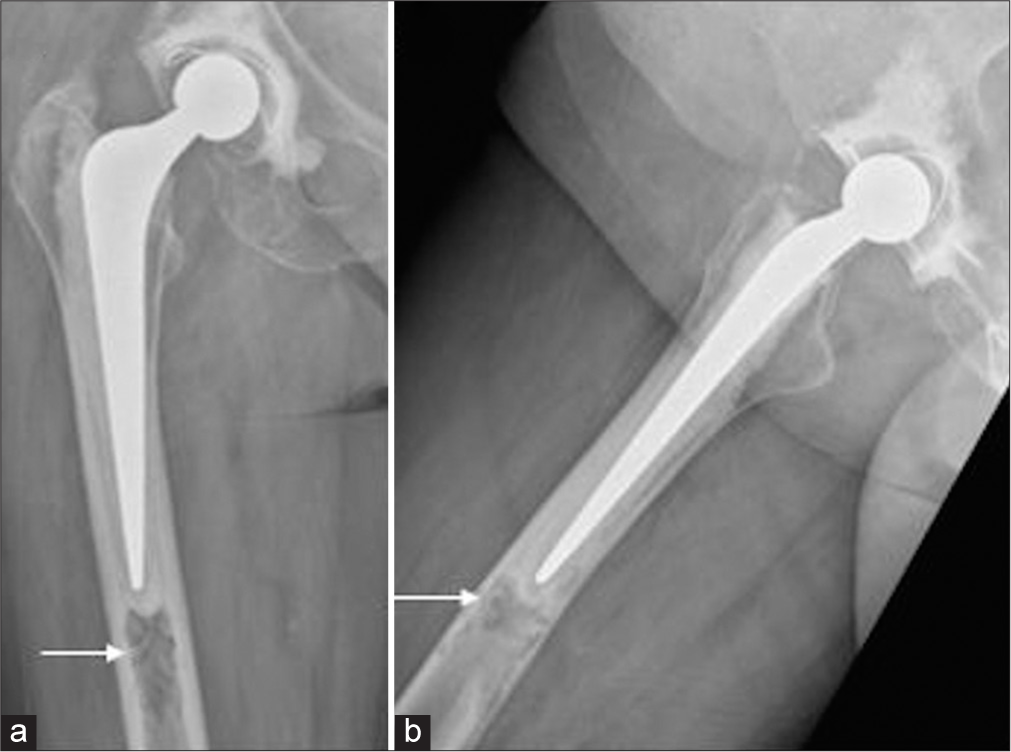
- Anteroposterior (a) (white arrow) and lateral (b) radiographs of the right hip performed at presentation 13 years post-total hip replacement demonstrating a lytic lesion in the femur adjacent to the tip of the femoral prosthetic stem (white arrow).
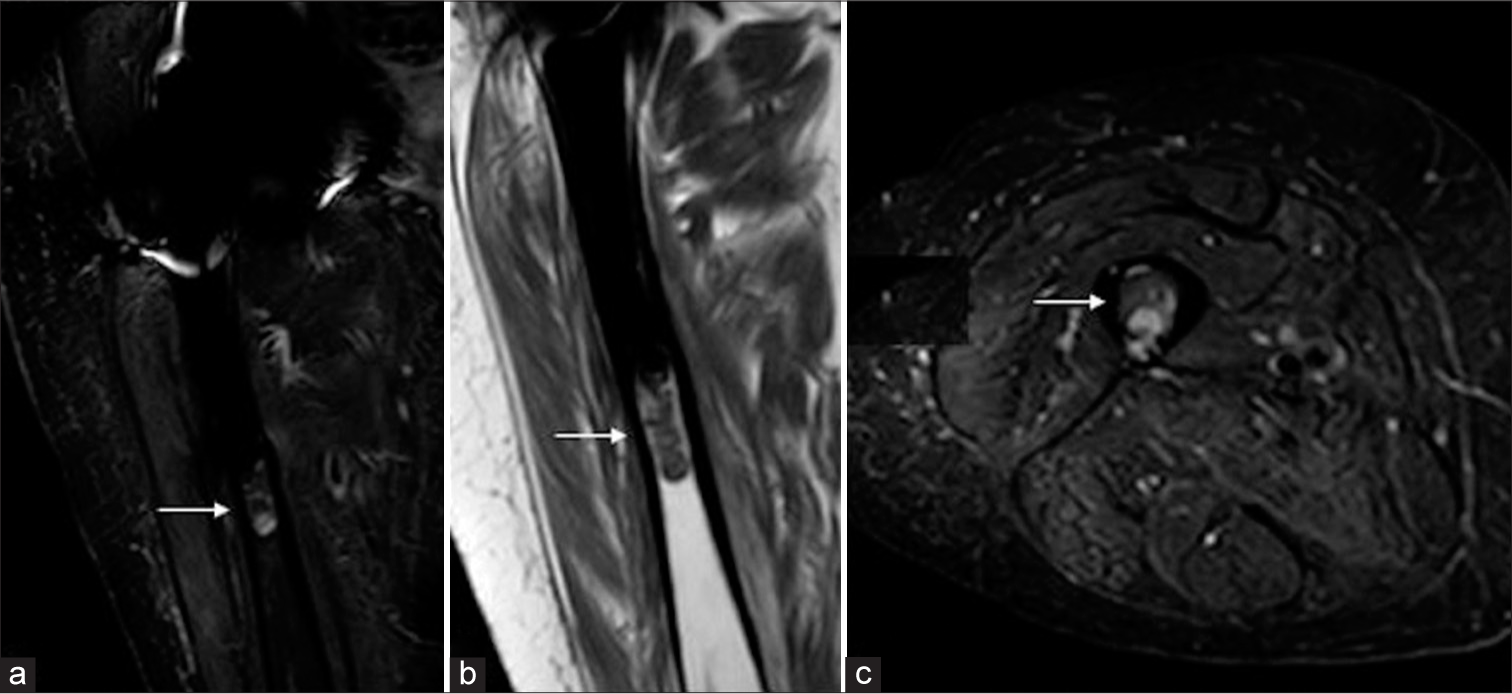
- (a) Coronal proton density fat saturation (white arrow), (b) coronal T1 (white arrow), and (c) axial proton density fat saturation (PDFS) weighted images obtained at the time of presentation showing abnormality distal to the femoral prosthesis (white arrow).
Prior X-rays from approximately 12 months after the right THR revealed that this lytic focus was a longstanding finding, with mild interval enlargement between the previous and the current radiographs. This was, however a new finding compared to post-operative radiographs obtained immediately after the surgery [Figure 5].

- (a and b) Anteroposterior and lateral views of the right hip performed immediately after the right total hip replacement as part of routine follow-up. Note the absence of the lytic lesion on these radiographs.
Given the relative long-term stability of the lesion (over approximately 13 years), this was thought to most likely represent osteolytic change involving a biodegradable osseous implant inserted at the time of the THR surgery. Taking this, as well as the patient’s advanced age, into account, she was conservatively managed with regards to her hip pain.
DISCUSSION
While peri-prosthetic osteolysis is a well-documented complication of total hip arthroplasty, this specific form of osteolysis due to the degradation of a restrictor is less common. Many different forms of cement restrictors, made of both artificial and biodegradable materials, are currently used for THR.[7] Degradation and osteolysis are complications usually seen with certain types of the latter. Two biodegradable restrictors, namely, the OptiPlug and SynPlug, have been specifically associated with this condition,[2,3,5] with safety notices issued regarding their use in some countries.[8] However, given the large number of THRs performed, we suspect that a substantial proportion of patients may already have these restrictions placed before the identification of this association.
Its focal morphology and gradual enlargement over time, when coupled with clinical and biochemical features of a potential malignancy, can result in this entity being mistaken for a neoplastic process. To further add to the confusion, neoplastic processes such as multiple myeloma and metastasis can present in the peri-prosthetic location, with nearly identical features on radiographs, CT, and MRI.[9,10]Due to the above factors, the distinction of the entity from malignancy based on a single set of imaging alone at the time of presentation is challenging. In some instances, bone scintigraphy would be a useful adjunct, as the absence of uptake at the site would make malignancy less likely, as was the case with our first patient. However, the osteolysis can be accompanied by an inflammatory response at the site, which can result in an increased accumulation of radiopharmaceuticals at the site, resulting in a false-positive finding.[11]
Hence, comparison with prior imaging is crucial in confirming benignity by virtue of the presence of the lesion over a prolonged period, in this case, 11 and 13 years, respectively. Where available, correlation with operative records would also be useful to confirm the use of the biodegradable cement restrictor in surgery if this has been documented. It is important to note, however, that the osteolysis associated with the cement restrictor would not be evident on routine radiographs performed immediately after the THR, as the degradation of the device begins to occur around two months after insertion, gradually progressing over the years.[2] As such, these cases are unusual given the long time intervals between the hip replacements and the presentation. This gradual progress in size may be a potential pitfall when attempting to distinguish this entity from malignancy. This would account for the increase in the size of lucency on the serial radiographs described in this paper. A particular distinguishing feature of this entity, as opposed to other neoplastic conditions, is that it is always seen in the same location at the distal tip of the prosthetic femoral stem, as this is where the restrictor plug is typically placed during the THR. [1]
Correct identification of this entity would prevent the patient from being subjected to unnecessary investigations for malignancy, which may include a bone biopsy and potential associated complications.
CONCLUSION
Periprosthetic osteolysis due to biodegradable cement restrictor can mimic malignancy, and clinicians need to be aware of this to avoid unnecessary investigations and biopsy.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent was not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using the AI.
Financial support and sponsorship
Nil.
References
- Cement restrictor function below the femoral isthmus. Clin Orthop Relat Res. 2007;458:111-6.
- [CrossRef] [PubMed] [Google Scholar]
- Osteolytic changes around biodegradable cement restrictors in hip surgery. Acta Orthop. 2016;87:239-44.
- [CrossRef] [PubMed] [Google Scholar]
- Osteolysis in cemented total hip arthroplasty involving the OptiPlug cement restrictor: More than an incident? Eur J Orthop Surg Traumatol. 2013;25:45-51.
- [CrossRef] [PubMed] [Google Scholar]
- Periprosthetic femoral fracture due to biodegradable cement restrictor. J Arthroplasty. 2012;27:1581.e13-5.
- [CrossRef] [PubMed] [Google Scholar]
- Osteolysis associated with optiplug bioabsorbable cement restrictors. J Bone Joint Surgery. 2011;93(Suppl 4):547-7.
- [Google Scholar]
- Society of Skeletal Radiology-white paper. Guidelines for the diagnostic management of incidental solitary bone lesions on CT and MRI in adults: Bone reporting and data system (Bone-RADS) Skeletal Radiol. 2022;51:1743-64.
- [CrossRef] [PubMed] [Google Scholar]
- The important role and choice of cement restrictor In: The well-cemented total hip arthroplasty. Berlin, Heidelberg: Springer; 2005. p. :150-4.
- [CrossRef] [Google Scholar]
- Urgent safety notice for SynPlug® and Optiplug® cement restrictors. 2014. Integra LifeSciences. Germany: Federal Institute for Drugs and Medical Devices; Available from: https://www.bfarm.de/SharedDocs/Kundeninfos/EN/11/2014/01674-14_kundeninfo_en.html [Last accessed on 2023 Feb 02]
- [Google Scholar]
- The imaging prevalence of osteolytic metastasis or multiple myeloma presenting as a periprosthetic lucency in the hip. AJR Am J Roentgenol. 2014;202:811-8.
- [CrossRef] [PubMed] [Google Scholar]
- Periprosthetic metastasis following total hip arthroplasty in a patient with lung carcinoma: A case report and review of literature. Medicine (Baltimore). 2019;98:e14071.
- [CrossRef] [PubMed] [Google Scholar]
- Nuclear medicine and the failed joint replacement: Past, present, and future. World J Radiol. 2014;6:446-58.
- [CrossRef] [PubMed] [Google Scholar]







