Translate this page into:
Post-traumatic hemorrhage in a large sacral Tarlov cyst causing acute radiculopathy

*Corresponding author: Jason Jacob, Department of Radiology, Queen Elizabeth University Hospital, Glasgow, Scotland, United Kingdom. jason.jacob1@nhs.net
-
Received: ,
Accepted: ,
How to cite this article: Jacob J, Gupta H. Post-traumatic hemorrhage in a large sacral Tarlov cyst causing acute radiculopathy. Indian J Musculoskelet Radiol. 2024;6:33-5. doi: 10.25259/IJMSR_56_2023
Abstract
Symptomatic Tarlov cysts (TCs) are an under-recognized clinical entity that should be considered in the differential for lower back pain. These are more common in women and can also be a cause of pelvic pain. Hemorrhagic TCs have been rarely reported in the literature, with symptoms ranging from lower back pain and radiculopathy to symptoms of cauda equina syndrome. We report on a female patient in her 50s who presented with radicular symptoms as a consequence of TC hemorrhage. Magnetic resonance imaging is the gold standard investigation, and this showed post-traumatic hemorrhage causing irritation of the sciatic nerve. Hemorrhagic TC is an important differential to consider in the setting of acute radicular pain, and the symptoms can be resolved with conservative management.
Keywords
Sciatica
Tarlov cysts
Radiculopathy
Hemorrhage
INTRODUCTION
Tarlov cysts (TCs) are most commonly found in the sacral region. These arise at the junction between the dorsal root ganglion and the nerve root and develop between the endoneurium and perineurium. It is postulated that TCs arise as a result of increased hydrostatic pressure in the canal, and cerebrospinal fluid accumulates in the nerve sheath.[1]
While TCs are a common incidental finding on magnetic resonance imaging (MRI), these are rarely symptomatic. Symptomatic TCs are an under-recognized clinical entity which should be considered in the differential diagnosis for lower back or radicular pain.[1] Here, we describe a case of hemorrhage into large sacral TCs causing acute neurological symptoms.
CASE REPORT
A female patient in her 50s was being investigated with pelvic ultrasound for perimenopausal symptoms and bloating. Ultrasound demonstrated complex bilateral adnexal masses [Figure 1].

- (a and b) Static images from a pelvic ultrasound study demonstrating complex, heterogeneously hypoechoic adnexal masses.
Further, evaluation of the adnexal lesions with MRI was warranted, and this revealed that the sonographic appearances were in fact due to multiple large lumbosacral TCs, largest at the bilateral S1 neural exit foramina (up to 7 cm on the right) causing widening of the foramina. These extended into the pelvic cavity giving the impression of adnexal masses [Figure 2].
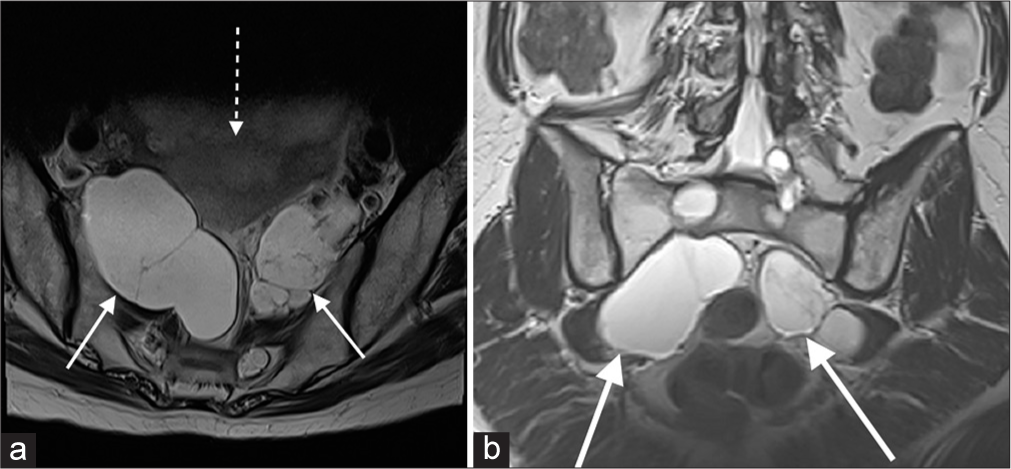
- (a and b) T2-weighted imaging demonstrating bilateral sacral Tarlov cysts (solid white arrows), either side of the uterus (dotted arrow), accounting for the sonographic findings.
The imaging findings remained stable for 2 years; however, after a fall, the patient developed acute radicular symptoms with shooting pain in the right buttock which radiated down the right leg. MRI scan performed for acute symptoms showed new fluid-fluid levels and heterogeneous signal changes within a right-sided sacral TC, most consistent with hemorrhage. There was associated edema and thickening of the adjacent right-sided sciatic nerve consistent with neural irritation [Figure 3].
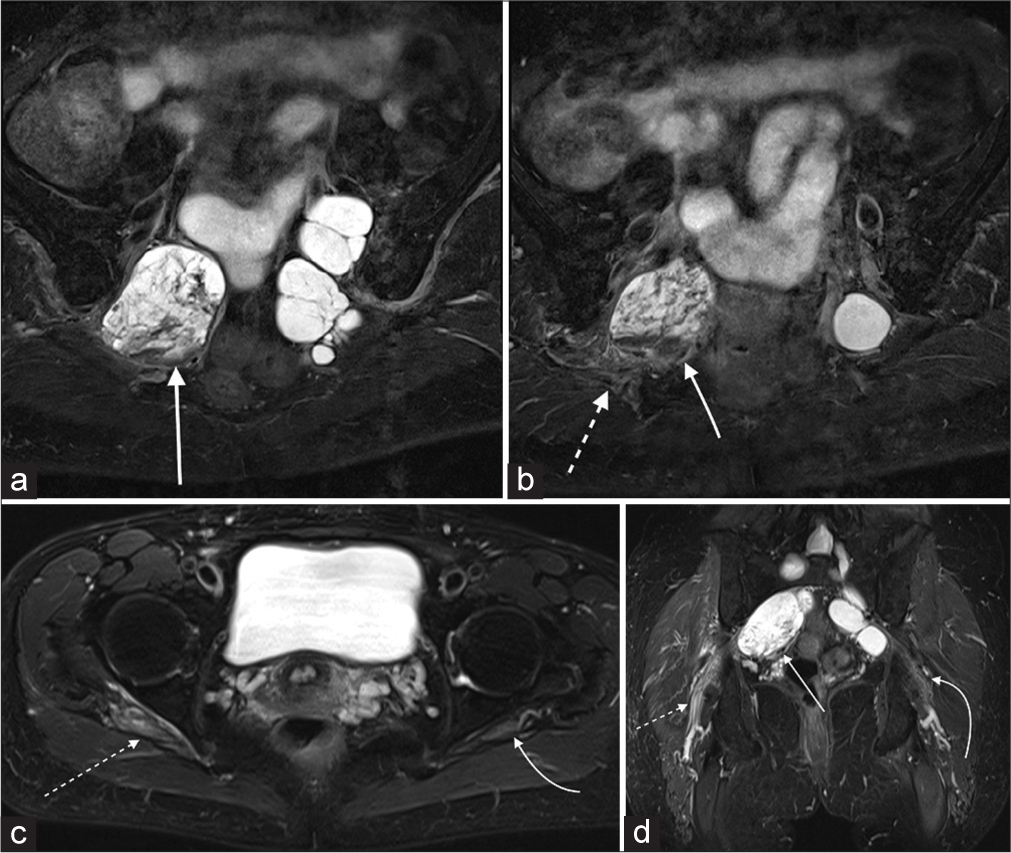
- (a-d) Fat-saturated T2-weighted imaging demonstrates low signal and fluid-fluid levels in a right-sided Tarlov cyst (solid white arrows) in keeping with hemorrhage. Dotted white arrows show edema and thickening of the right sciatic nerve; curved arrows show normal left sciatic nerve.
The case and the imaging findings were discussed at a spinal multidisciplinary team meeting, and the symptoms were attributed to post-traumatic hemorrhage into a right-sided TC following trauma. The symptoms were resolved with conservative management.
DISCUSSION
TC formation is related to hydrostatic pressure, and this is the highest in the lower lumbar and sacral spine.[1] Radicular pain and paresthesia may be experienced with TCs due to irritation of the dorsal ganglion, which predominantly contains sensory neural components.[1,2] If the cysts enlarge in size significantly, these may compress the motor fibers in the ventral roots, causing weakness resulting in absent Achilles tendon reflexes, weak ankle movements, and can also cause bladder or bowel disturbance.[1,2]
Hemorrhage into TCs has been rarely reported in the literature, with symptoms ranging from acute lower back pain, radiculopathy, leg weakness, perineal numbness, and urinary retention[3-5]. It has been postulated that the symptoms may occur as a result of further increase in pressure within the cyst, which may compound pressure-related effects within the adjacent nerve roots.[4,5] In the acute setting, in patients with known TCs, hemorrhage into the cysts should, therefore, be a differential diagnosis for cauda equina syndrome. As illustrated in this case, MRI is the optimal modality that can accurately detect and characterize cyst hemorrhage, compression, and inflammation of adjacent nerve roots.
Symptomatic TCs have been identified more commonly in women.[6,7] Abdominal and pelvic pain have also been reported with TCs,[8] and the patient may be investigated with ultrasound in the first instance. As in our case, it is important to be aware that large TCs can mimic adnexal cysts or masses. Kim et al.[9] report a case of TCs that were misdiagnosed as adnexal cysts and treated with sclerotherapy, leading to a chemically-induced cauda equina syndrome. TCs are, therefore, in the differential for large adnexal cysts, and MRI evaluation should be considered before any intervention.
The management of symptomatic TCs is a subject of debate. In our case, the patient was managed conservatively; however, percutaneous cyst aspiration, fibrin glue injection or, surgical cyst resection, or cyst fenestration are the other potential treatment options with symptom improvement reported in the literature.[2,6,10]
CONCLUSION
TCs can rarely be symptomatic, and these are an under-recognized clinical entity. It is important to consider this in the differential for pelvic and lumbar pain, and these can mimic adnexal cysts. It is important to be aware of the complication of hemorrhage into TCs, which can present as acute radiculopathy (as in our case), or present with symptoms of cauda equina syndrome, which has been rarely reported in the literature. MRI is the modality of choice in the diagnosis and evaluation of large cysts and complications such as hemorrhage and perineuritis.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent is not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Symptomatic tarlov cysts are often overlooked: Ten reasons why-a narrative review. Eur Spine J. 2019;28:2237-48.
- [CrossRef] [PubMed] [Google Scholar]
- Haemorrhagic tarlov cyst: A rare complication of anticoagulation therapy. Oxf Med Case Reports. 2021;2021:omab063.
- [CrossRef] [PubMed] [Google Scholar]
- Incomplete cauda equina syndrome secondary to haemorrhage within a tarlov cyst. BMJ Case Rep. 2017;2017:r-219890.
- [CrossRef] [PubMed] [Google Scholar]
- Tarlov cyst hemorrhage causing acute radiculopathy: A case report. Clin Neuroradiol. 2018;28:123-5.
- [CrossRef] [PubMed] [Google Scholar]
- Tarlov cysts: An overlooked clinical problem. Semin Musculoskelet Radiol. 2011;15:163-7.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of simple and complex sacral perineural Tarlov cysts in a French cohort of adults and children. J Neuroradiol. 2017;44:38-43.
- [CrossRef] [PubMed] [Google Scholar]
- Presacral tarlov cyst as an unusual cause of abdominal pain: New case and literature review. World Neurosurg. 2018;110:79-84.
- [CrossRef] [PubMed] [Google Scholar]
- Tarlov cysts misdiagnosed as adnexal masses in pelvic sonography: A literature review. Front Med (Lausanne). 2020;7:577301.
- [CrossRef] [PubMed] [Google Scholar]
- Tarlov cysts: A study of 10 cases with review of the literature. J Neurosurg. 2001;95:25-32.
- [CrossRef] [PubMed] [Google Scholar]






