Translate this page into:
A rare case of acute traumatic complicated right axillary artery pseudoaneurysm with quadrangular space syndrome

*Corresponding author: Santhosh Reddy Agumamidi, Department of Radiology, Amandeep Hospital, Amritsar, Punjab, India. sandyagumamidi@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Agumamidi SR, Agrawal P. A rare case of acute traumatic complicated right axillary artery pseudoaneurysm with quadrangular space syndrome. Indian J Musculoskelet Radiol. 2024;6:70-4. doi: 10.25259/IJMSR_33_2023
Abstract
Axillary artery pseudoaneurysms are relatively rare, with few reported cases found in the literature. There have been high rates of rupture and compression-related complications in trauma-related pseudoaneurysms of the upper limb. Prompt diagnosis with non-invasive imaging modalities such as ultrasound, magnetic resonance imaging, and computed tomography. Angiography is required for immediate intervention and prevention of complications. Here, we present a case of an extremely rare right-sided acute traumatic axillary artery pseudoaneurysm with compression, resulting in quadrangular space syndrome in a 31-year-old male patient. We performed a critical literature review of the same and identified only a few previously reported cases.
Keywords
Axillary pseudoaneurysm
Quadrangular space syndrome
Magnetic resonance imaging shoulder
INTRODUCTION
Axillary artery pseudoaneurysms occur very rarely following acute shoulder trauma. Only a few case reports have been published in the literature. In the cases of blunt trauma, the prevalence of axillary artery pseudoaneurysm is around 0.3%.[1] A pseudoaneurysm is an enclosed pulsatile thin-walled vascular abnormality bounded only by tunica adventitia with a wide or narrow neck connecting the parent feeding artery in contrast to a true aneurysm, which is bounded by all three layers of the arterial wall. The major etiologies of pseudoaneurysms are traumatic and iatrogenic. Axillary artery pseudoaneurysms, in particular, are usually caused by acute shoulder trauma, most associated with complex displaced skeletal trauma such as humerus neck fractures and glenohumeral joint dislocations. Iatrogenically, they can occur during catheter-related intra-arterial procedures. Clinically, it is diagnosed as a slowly growing palpable soft mass, depending on the size, with a discernible pulsation/thrill within the axillary fossa. If neglected, these pseudoaneurysms may lead to complications such as intraluminal thrombosis, rupture, distal arterial migration of emboli, distal ischemia due to vascular flow steal, and compression of surrounding neural/vascular tissues, depending on their location.
CASE REPORT
A 31-year-old right-handed male presented to the emergency unit with a right shoulder injury after a motorcycle crash that resulted in an auto-rickshaw running over his right shoulder region. On arrival, the patient’s pulse rate was 88 beats/min, blood pressure was 136/80 mmHg, and the respiratory rate was 16 breaths/min. The patient was conscious and oriented in time and space, with bruises over the right shoulder area. He reported severe pain, tenderness, and inability to move his right shoulder, with abduction being severely compromised. On clinical examination, there was no significant palpable mass/hematoma in the axillary region. The right axillary, brachial, ulnar, and radial pulses were normal at the time of examination. The patient was shifted to the orthopedic unit and later for a right shoulder joint X-ray. No fracture was detected on the right shoulder radiographs. The patient was admitted for further management in view of severe right shoulder pain and profound restriction on movement of the limb. Post 24 hours of admission. The concerned orthopedic resident doctor clinically could palpate a pulsatile growing deep-seated mass within the right axilla with worsening pain and the inability to shoulder movement. On suspecting a possible vascular injury with hematoma and to rule out any major rotator cuff injury, the patient was shifted to the magnetic resonance imaging (MRI) department for shoulder imaging. The scan procedure was suboptimal due to severe pain complained by the patient and owing to motion artifacts. Computed tomography angiography (CTA) could not be performed as the patient had an allergic reaction to iodine-based contrast in the past.
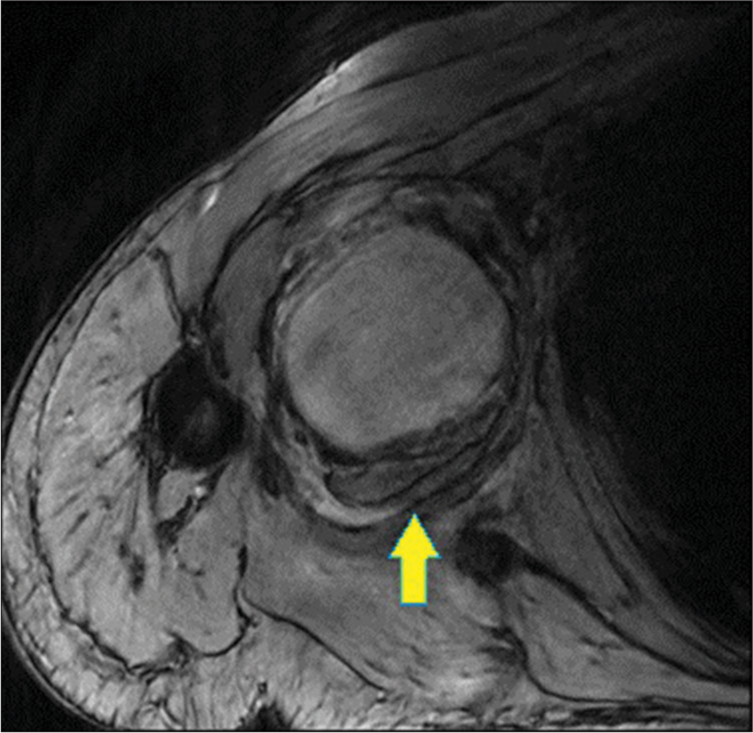
The right shoulder MRI imaging findings showed a large 6.9 × 6.4 × 5.6 cm sized lesion with central T1 and T2 flow void measuring approximately 3.7 × 4.8 × 4.6 cm in the right axillary region. The walls of the lesion appeared significantly thickened, organized, whorled, and T2 hyperintense. The lesion was seen located within the right intermuscular axillary space interposed between the subscapularis and teres minor muscle. The axillary artery was coursing in proximity along the anterior margin of the lesion. A definite vascular connection of the lesion with the axillary artery could not be demonstrated on the suboptimal MRI images. These findings were suggestive of partial peripherally thrombosed traumatic pseudoaneurysm of the right axillary artery [Figures 1-3].

- T2 sagittal image showing central flow-related signal void within the pseudoaneurysm (Yellow Arrow).
- Axial GRE image with central intraaneurysmal liquid blood with thick surrounding blooming from partial peripherally thrombosed lumen (Yellow arrow).
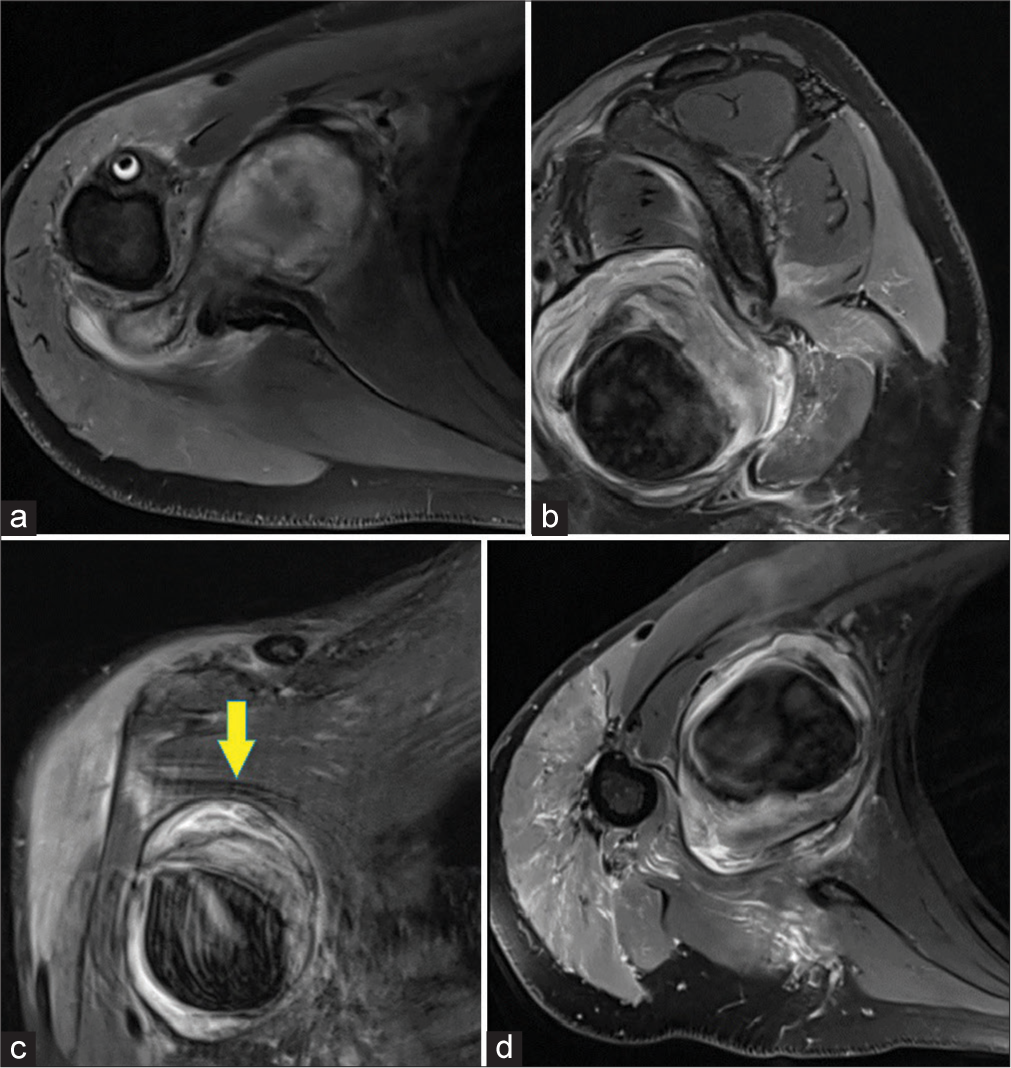
- Multiplanar proton density fat saturation images - (a and d) axial, (b) sagittal, (c) coronal, depicting large peripheral partially thrombosed pseudoaneurysm (Yellow arrow in c) in the intermuscular axillary space. However, no definite vascular feeding neck could be demonstrated on magnetic resonance imaging.
Marked proton density fat saturation (PDFS) hyperintense soft-tissue and peri-neurovascular edema were seen along the posterior aspect of the above-mentioned pseudoaneurysm, causing severe compromise of the quadrangular space. There was an associated diffuse short tau inversion recovery (STIR)/PDFS hyperintense signal within the deltoid and teres minor muscles likely suggestive of traumatic axillary nerve neuropathy (quadrilateral space syndrome) [Figures 4 and 5].
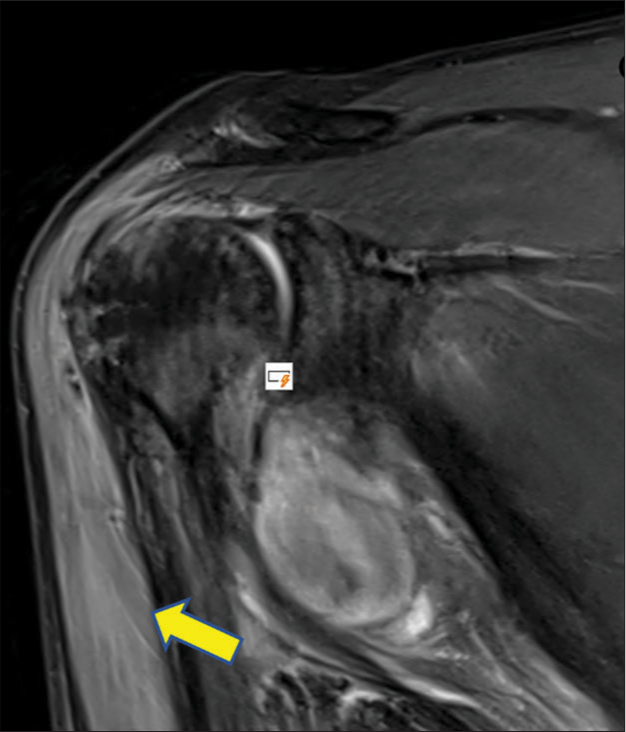
- Coronal proton density fat saturation images showing hyperintense signal within the bulk of deltoid (Arrow) muscle hinting at traumatic axillary neuropathy due to quadrilateral space syndrome.
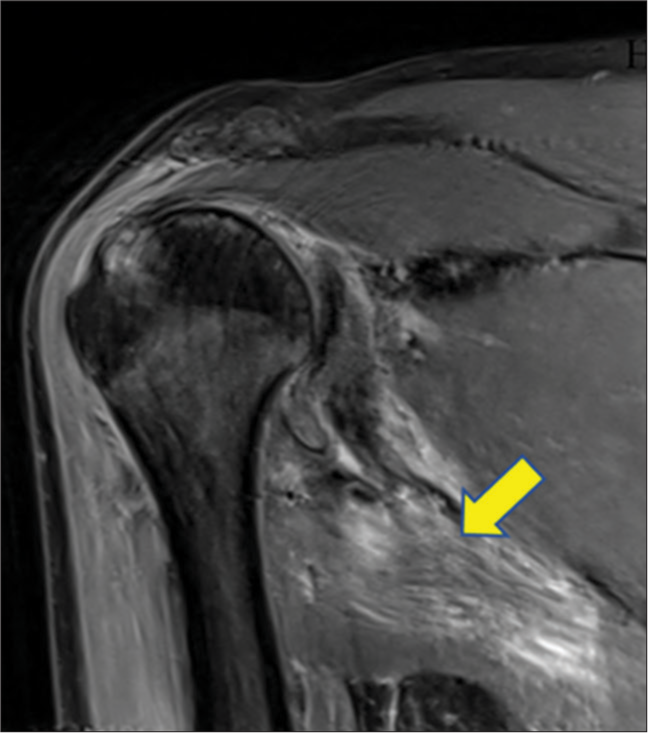
- Coronal proton density fat saturation images showing hyperintense signal within the bulk of teres minor (arrow) muscle hinting at traumatic axillary neuropathy due to quadrilateral space syndrome.
Diffuse edema of the supraspinatus tendon with a thin intrasubstance tear was noted at the site of insertion.
After the MRI scan, a screening ultrasound (USG) of the right shoulder region was done that depicted a peripherally thrombosed pulsatile pseudoaneurysm within the axillary space [Figure 6a and b] and a demonstrable thin vascular communication with the right axillary artery [Figure 6c and d]. No other mass or hematoma was detected.
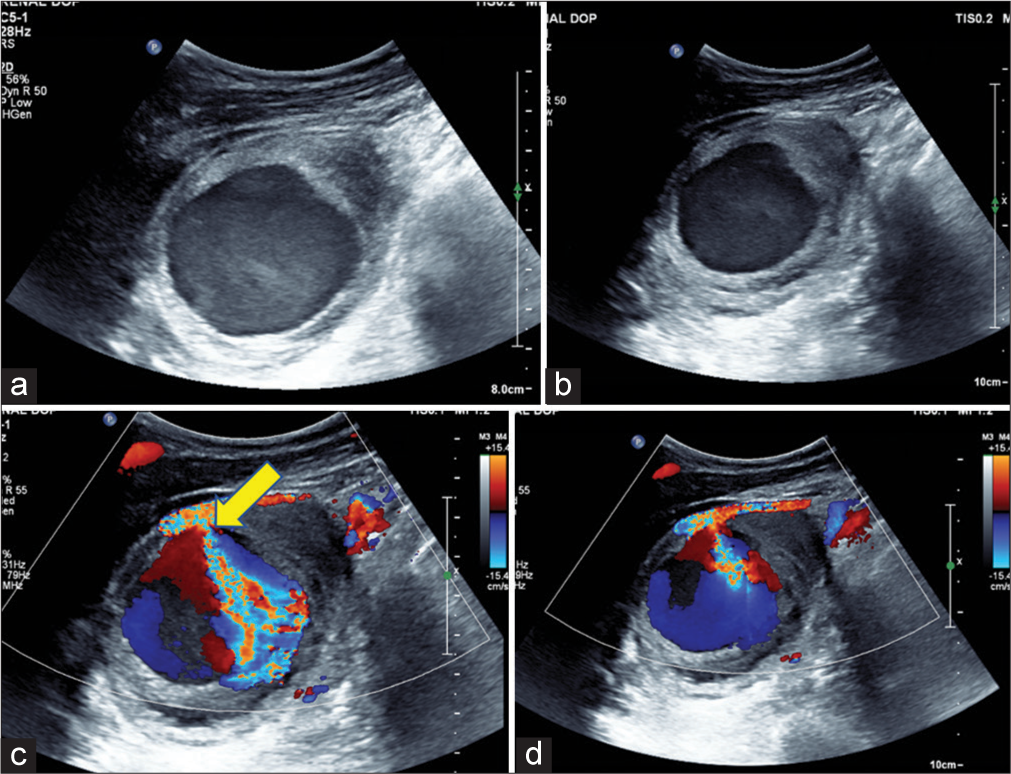
- (a and b) Screening ultrasound B-mode and (c and d) Doppler images of the right shoulder region depicting a peripherally thrombosed pulsatile pseudoaneurysm with luminal Yin-Yang sign (c and d) within the axillary space and a demonstrable thin vascular communication (yellow arrow in 6c) with the right axillary artery.
For further management, the patient was referred to a higher center in a different hospital and was given percutaneous USG-guided thrombin injection into the pseudoaneurysm.
DISCUSSION
Pseudoaneurysms are rare vascular wall abnormalities. Depending on location, local mass effect may result in neural, vascular, or airway compression.[2] Specifically, when we speak of upper limb arteries such as axillary arteries, as in our case, pseudoaneurysms are relatively rare in occurrence following trauma. Several instances of pseudoaneurysms appear silent on initial clinical examination. Regular follow-up examinations are needed to suspect a slow-growing pseudoaneurysm and intervene immediately to avoid compression of the brachial plexus.[3]
Pseudoaneurysm, as the name suggests, is a false aneurysm arising from the arterial wall when it is weakened by trauma or infection. Its wall does not contain all the layers of an artery like that of a true aneurysm, resulting in rupture if neglected.[4] The axillary artery is susceptible to trauma owing to its fixed anatomical position between the anterior and posterior circumflex arteries and scapular arteries. Furthermore, the humeral head movement compresses the axillary artery against the pectoralis minor.[5]
Clinically unnoticed pseudoaneurysm can be fatal and can lead to several complications such as rupture, nerve compression, and thrombosis. When a pseudoaneurysm is clinically suspected, imaging modalities, such as USG examination, CTA, magnetic resonance angiography, or digital subtraction angiography (DSA), may be useful to assist in the diagnosis.[6] The USG is relatively inexpensive and portable and can demonstrate a feeder neck of pseudoaneurysm. However, it is operator-dependent and cannot generate detailed 3D vascular images required for intervention planning. CTA and DSA provide excellent vascular anatomical detail and are also operator-independent; however, with radiation exposure and its contraindications in patients with renal failure and contrast allergy. DSA has the benefits of simultaneous therapeutic interventions such as ballooning and pseudoaneurysm coiling. MRI is another non-invasive modality that provides excellent soft-tissue detailing and vascular delineation. The disadvantages of MRI are that the scan is time-intensive, expensive, and images that are highly susceptible to metallic object-derived artifacts.[7] In our patient who had a history of iodine contrast allergy, only USG and MRI remain as the two possible diagnostic modalities.
Several options for intervention are used in clinical practice depending on availability and radiologist expertise. The more traditional method of USG-guided compression carries its disadvantages, such as patient discomfort and limited accessibility due to overlying clavicular bone when it comes to axillary artery pseudoaneurysms. Minimally invasive percutaneous thrombin is preferred over DSA-guided embolization/stent placement as the latter poses a challenge from the tortuous course, multiple branches arising from axillary and subclavian arteries, many flexion points, and requirement of long-term monitoring of stent-graft from re-stenosis. Few cases of wide-necked aneurysms are treated with success using a combination of thrombin injection and balloon occlusion. In cases of large growing aneurysms causing severe nerve compression and in which those mentioned above minimally invasive interventions fail, surgical exploration/decompression is effective.[8]
In our case, early diagnosis in the emergency department on patient arrival could not be made, as there was no clinically palpable soft-tissue mass/hematoma within the right axilla. Furthermore, the patient was hemodynamically stable with no comorbidities. His only complaints were severe right shoulder pain and moderate inability to shoulder movement. However, during admission approximately 24 h later, clinical examination revealed a growing palpable pulsatile mass in the right axilla along with completely worsened shoulder movements. As a result of good communication between the clinical orthopedic unit and our radiology department, the patient was immediately shifted for an MRI.
Quadrilateral/quadrangular space syndrome is the compression of neurovascular structures in the quadrilateral space of the shoulder. The quadrangular (or quadrilateral) space is located along the posterolateral aspect of the shoulder. It is bounded by the teres minor superiorly, the teres major muscle inferiorly, the long head of the triceps brachii muscle medially, and the humeral surgical neck laterally. The quadrilateral space serves as a corridor for the axillary nerve and posterior humeral circumflex artery. Although rare, quadrilateral space pathologies comprise mainly nerve compression due to repetitive stress usually seen in young athletes and laborers.[9]
The etiology of pseudoaneurysm is shoulder trauma in our case. MRI is the modality of choice for the diagnosis of our patient, who had an allergy to iodine-based contrast agents and clinical signs of nerve compression. MRI demonstrates hyperintense signals within teres minor and/or deltoid muscles on proton density/STIR sequences in acute settings. Few chronic and neglected cases can show atrophy and fatty infiltration within these muscles.[10]
CONCLUSION
Trauma to axillary neurovascular structures is significantly rare. Prompt clinical examination, timely diagnostic imaging, and meticulous follow-up for complications are needed for rapid and reliable management reducing the delay before repair. Neglected axillary trauma-related pseudoaneurysms can lead to local compression-related complications such as axillary neuropathy, rupture and hematoma formation, distal embolization, and distal ischemia. Imaging modalities useful are Doppler USG, DSA, CTA, and MRI when evaluating axillary injury. A screening brachial plexus MRI can be done to rule out brachial plexus injury. Treatment options available are USG-guided percutaneous thrombin injection and DSA endovascular techniques such as balloon occlusion/stenting and pseudoaneurysm coiling.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent is not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Vascular complications of simple anterior dislocations of the shoulder. Three cases. J Ann Chir. 1982;36:329-33.
- [Google Scholar]
- Iatrogenic subclavian artery pseudoaneurysm causing airway compromise: treatment with percutaneous thrombin injection. J Vasc Surg. 2004;40:371-4.
- [CrossRef] [PubMed] [Google Scholar]
- Delayed rupture of a pseudoaneurysm in the brachial artery of a burn reconstruction patient. World J Emerg Surg. 2013;8:21.
- [CrossRef] [PubMed] [Google Scholar]
- Amputation for upper extremity ischemia following shoulder dislocation: Case report and a review of dhanliterature. Eur Res J. 2015;1:66.
- [CrossRef] [Google Scholar]
- An unusual presentation of traumatic pseudoaneurysm of axillary artery mimicking soft tissue tumor. J Surg Case Rep. 2012;2012:17.
- [CrossRef] [PubMed] [Google Scholar]
- Management of traumatic arterial pseudoaneurysms as a result of limb trauma. Formos J Surg. 2016;49:89-100.
- [CrossRef] [Google Scholar]
- Pseudoaneurysms and the role of minimally invasive techniques in their management. Radiographics. 2005;25(Suppl 1):S173-89.
- [CrossRef] [PubMed] [Google Scholar]
- Peripheral nerve injury associated with shoulder trauma: A retrospective study and review of the literature. J Clin Neuromuscul Dis. 2002;4:1-6.
- [CrossRef] [PubMed] [Google Scholar]






