Translate this page into:
Spondylocostal dysostosis: A rare case report

*Corresponding author: Neha Bagri, Associate Professor, Department of Radiodiagnosis, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi, India. drnehabagri@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kamodia AS, Senthilkumar SS, Bagri N. Spondylocostal dysostosis: A rare case report. Indian J Musculoskelet Radiol. 2023;5:154-7. doi: 10.25259/IJMSR_45_2023
Abstract
Spondylocostal dysostosis (SCD), also known as Jarcho Levin syndrome, is a rare congenital dysostosis characterized by multiple congenital vertebral and rib anomalies. The child usually presents with respiratory distress at birth with eventual development of short trunk dwarfism. Associated congenital anomalies are rare; however, they need evaluation. We report a 6-month-old Indian girl with SCD who presented with respiratory distress and an asymmetrical small thoracic cavity. The diagnosis was made with radiographs, computed tomography scans, and magnetic resonance imaging (MRI) showing multiple rib and vertebral segmentation anomalies. We would also highlight the importance of MRI in these patients and illustrate other associated brain and spine anomalies.
Keywords
Spondylocostal dysostosis
Congenital
Vertebral
Rib anomalies
Magnetic resonance imaging
INTRODUCTION
Spondylocostal dysostosis (SCD) is a rare skeletal dysplasia, first described by Jarcho and Levin in 1938.[1] Multiple congenital vertebral and rib anomalies, short neck and trunk, abnormal segmentation of the spine and ribs, and normal-length limbs manifest the disease condition. The anomalies include overgrown, fused or missing ribs and segmentation defects of the vertebrae such as fusion, hemivertebrae, or block vertebrae. Other associated congenital anomalies are rare; however, they need evaluation.[2] The exact prevalence of SCD is not well-established, but it is considered an extremely rare condition.[3] Here, we describe the clinical presentation and imaging characteristics of a 6-month-old female child with SCD who presented with respiratory distress at birth.
CASE REPORT
A 6-month-old female child was referred to the pediatric clinic with a history of respiratory distress since birth. The child was born at full-term through an elective cesarean section through an uneventful pregnancy and delivery. There was no significant family history of consanguinity among the parents. The parents reported rapid breathing and retractions in the first hours of life. The thorax appeared asymmetrical and showed limited chest expansion during inspiration, with evident retractions of the left hemithorax with each breath and increased respiratory effort [Figure 1]. The child’s vital signs were within the normal range, except for tachypnea. On auscultation, reduced breath sounds were noted over the left hemithorax, suggesting hypoventilation. Palpation of the thorax revealed mild scoliosis and rib abnormalities. These clinical features raised suspicion for congenital skeletal dysplasia. The child was sent to the Department of Radiology for further evaluation.
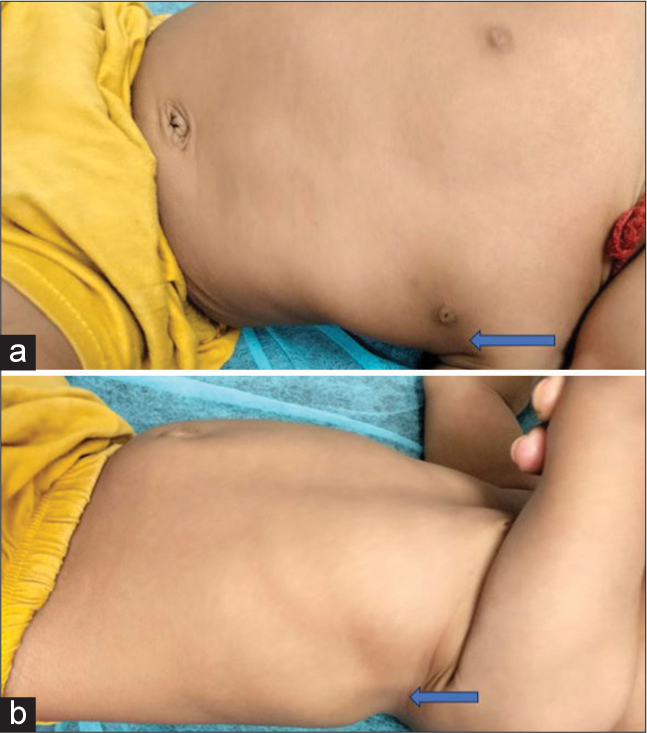
- (a and b) Clinical pictures of the child show an asymmetrical small thorax with a clinically palpable defect in the left-sided chest wall (blue arrow).
Radiological investigations were performed to assess the skeletal anomalies. Antero-posterior and lateral radiographs of the thorax and spine were obtained. The X-rays revealed abnormalities of the ribs and thoracic spine and mild thoracic dextroscoliosis. There was an absence of the left 4th–6th ribs. Furthermore, there were segmentation defects of the thoracic vertebrae in the form of hemivertebrae [Figure 2]. The vertebral and rib anomalies were consistent with the diagnosis of SCD. In addition, there was dextroposition of the heart. The rest of the skeletal survey revealed no abnormalities.

- Anteroposterior X-rays of the thorax and spine show abnormalities of the ribs and thoracic spine with mild thoracic dextroscoliosis. Note the absence of the left 4th–6th ribs and segmentation defects of the thoracic vertebrae in the form of hemivertebrae.
A computed tomography (CT) scan of the thorax and spine was performed to obtain more detailed imaging of the skeletal and, if any, associated cardiac abnormalities. The CT images confirmed thoracic dextroscoliosis and the presence of hemivertebrae with asymmetrically fused vertebral bodies. However, no bony spinal canal stenosis was noted. There was an absence of the left 4th–6th ribs with abnormally short and fused ribs, contributing to the thoracic cage deformities observed on clinical examination. In addition, there was a dextroposition of the heart; however, no congenital cardiac anomalies were seen [Figure 3].

- Computed tomography (CT) scan of the thorax and spine. (a) Showing the absence of the left 4th–6th ribs leading to the thoracic cage deformity (green arrow) and vertebral anomalies (yellow arrow). (b) Showing dextroposition of the heart. (c and d) 3D CT images confirming multiple rib and vertebral anomalies (green arrow).
MRI of the brain and spine was done to rule out associated congenital anomalies. It showed a low lying and tethered cord with filum terminale lipoma. There was associated dorsolumbar short segment syrinx and sacral spinal meningeal cysts type III (arachnoid cysts) [Figure 4].

- Magnetic resonance imaging of brain and spine. (a and b) T2W sagittal and axial images showing low-lying and tethered cord (red arrow) with associated dorso-lumbar short segment syrinx (yellow arrow), (c and d) T1W axial and sagittal images showing filum terminale lipoma (green arrow).
DISCUSSION
SCD is characterized by abnormal segmentation and formation of the spine and rib. There is resultant mild congenital scoliosis with moderate thoracic insufficiency, and most of the affected children survive till adulthood. It usually shows autosomal recessive inheritance and is associated with DLL3 gene mutation. The main clinical and radiological differential diagnosis is spondylothoracic dysostosis (Lavy– Moseley syndrome).[3] This can be differentiated with the help of certain imaging features [Table 1].
| Spondylocostal dysostosis | Spondylothoracic dysostosis | |
|---|---|---|
| Rib anomalies | Fused, missing, or overgrown ribs | Posterior fusion of ribs (Shows crab-like configuration) |
| Spine anomalies | Fusion, hemivertebrae, or block vertebrae | Cervicothoracic fusion or fusion of occiput and C1 |
| Associated congenital anomalies | Rare; however, neural tube defects can be seen | More common, including neural tube defects, anorectal malformations |
| Distribution | Worldwide | 50% from Puerto Rico |
| Clinical course | Most survive into adulthood | High infant mortality rate |
SCD and its association with neural tube defects have been frequently reported in the literature. It has been postulated that the vertebral anomalies observed in this syndrome are secondary to a developmental disturbance between the 4th and 8th weeks of gestation, as multiple centers of chondrification form at that time around the notochord to form a complete cartilaginous pro-vertebra. Failure of these chondrification centers to develop or unite can result in hemivertebrae or butterfly vertebrae with anomalous rib development secondary to anomalous vertebral development.[4]
There are multiple surgical treatments described for SCD, such as vertical expandable prosthetic titanium ribs (VEPTR) and chest wall reconstruction with latissimus dorsi flap transfers for thoracic insufficiency. The treatment depends on the degree of thoracic insufficiency, concurrent pulmonary complications, and chest wall defects aimed at improving quality of life. In patients with chest wall defects such as herniation of thoracic contents or paradoxical chest wall movements during respiration, the use of a latissimus dorsi flap improves respiratory function and decreases the rate of infections. VEPTR manages the issue of thoracic insufficiency better than the latissimus dorsi flap. The goal of VEPTR is to improve scoliotic curves and expand thoracic volume, hence helping to create space for lung development. In VEPTR, one or more vertically oriented distracting devices are attached superiorly to the ribs and inferiorly to the ribs, spine, or pelvis and are serially lengthened as the child grows. However, close clinical follow-up with these patients is recommended, particularly early on in life, considering the high rates of infant mortality observed. The ideal time to operate should maximize growth potential and minimize respiratory morbidity. This time frame remains undetermined. If a significant decline in function and respiratory status or failure to thrive is observed, then surgical intervention with VEPTR should be considered.[5]
CONCLUSION
This case report highlights the importance of considering SCD in a child with small thorax and respiratory distress. Cross-sectional imaging plays a crucial role in better delineating the osseous and other associated craniospinal anomalies. Restrictive lung disease is the key factor determining the quality of life and span, thus requiring apt management.
Acknowledgments
We wish to thank the Department of Radiodiagnosis, VMMC and Safdarjung Hospital staff for their support and cooperation.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Hereditary malformations of the vertebral bodies. Bull Johns Hopkins Hospital. 1938;62:216-26.
- [Google Scholar]
- Jarcho-Levin syndrome: A rare case of thoracic insufficiency syndrome in a newborn. Indian Pediatr Case Rep. 2023;3:171-3.
- [CrossRef] [Google Scholar]
- The clinical and radiological distinction between Spondylothoracic dysostosis (LavyMoseley Syndrome) and Spondylocostal dysostosis (Jarcho-Levin syndrome) Pediatr Radiol. 2010;41:384-8.
- [CrossRef] [PubMed] [Google Scholar]
- Spondylocostal dysostosis (Jarcho-Levine syndrome) associated with occult spinal dysraphism: Report of two cases. J Pediatr Neurosci. 2015;10:127-32.
- [CrossRef] [PubMed] [Google Scholar]
- Spondylocostal dysostosis: A literature review and case report with long-term follow-up of a conservatively managed patient. Case Rep Orthop. 2018;2018:1795083.
- [CrossRef] [PubMed] [Google Scholar]







